Antiemetic Drugs
Antiemetic drugs are used to suppress emesis, or vomiting. These drugs are discussed here because vomiting is often a symptom of severe vertigo, and thus a common clinical presentation during the acute phase of a vestibular disorder. While patients do not report for balance function testing in this distressed state (e.g., the acute phase of a peripheral vestibular lesion), some will still be managed medically by the use of antiemetic drugs when they are seen in the balance clinic. It is therefore important to understand these drugs and to be able to recognize common brand and generic names in patient charts.
How They Work 1
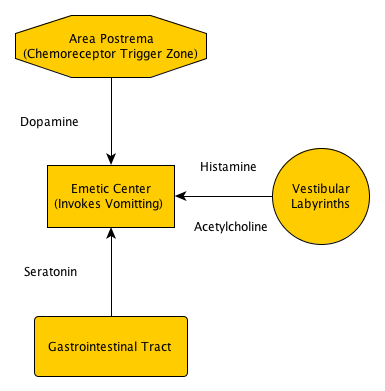
FIGURE 1 (adapted1)
To understand how these drugs work, you must get to know the emetic center of the central nervous system: the areas of the reticular formation in the brain stem that regulate vomiting. Keep in mind the emetic center is not a discrete nucleus, but rather a diverse system. There are three major afferent sources that carry the emetic signal to the brain stem to induce vomiting (figure 1): the chemoreceptor trigger zone (CTZ) in the area postrema, the visceral afferents from the gastrointestinal (GI) tract, and vestibular afferents from the labyrinths.
- The Three Afferent Relays
- Chemoreceptor Trigger Zone
- Visceral Afferents
- Labyrinths
Each afferent pathway activates receptors to trigger emesis using different, pathway-specific neurotransmitters (figure 1). The CTZ releases dopamine (affecting D2 receptors); the GI tract uses seratonin (affecting 5HT3 receptors); and the vestibular afferents transmit histamine (affecting H1 receptors) and acetylcholine (affecting muscarinic receptors). In fact, it has been shown in rats that antagonist drugs appropriate for one pathway, for example antidopaminergics for the CTZ, do not prevent pica (rat analogue to emesis) when other emetic pathways are stimulated, such as the release of histamine from the labyrinthine relay.1
- Neurotransmitters Released
- Dopamine (D2 receptors)
- Seratonin (5HT3 receptors)
- Histamine (H1 receptors)
- Acetylcholine (muscarinic receptors)
That said, it is also possible to supress emetic signals from multiple pathways by using drugs that act on the emetic center itself (in the reticular formation). Diphenidol, for example, has been shown to be effective against emetic signals from several pathways, though its antiemetic action is uncertain at this time.


Common Uses 2
Antiemetics are used to suppress nausea and vomiting regardless of the underlying cause. You can assume therefore, correctly, that antiemetics treat only the symptoms (i.e., nausea and vomiting) - not the reason emetic signals are being relayed in the first place. That is not to reduce the utility or importance of these medications; in the face of such unpleasant symptoms patients are interested only in swift relief, which these medications can provide without establishing a detailed differential diagnosis.
As mentioned above, the neurotransmitters released by the three pathways are specific and independent of one another. Because antiemetics are selective in which receptors they block (e.g., antidopaminergics and antiserotonergics), these drugs can be prescribed based on the pathway likely responsible for the emetic signal. Conversely, using drugs that suppress activity in the emetic center directly can be used to suppress emesis from multiple pathways. Specific prescription and dosing strategies are not within the scope of this website, but the following are general practices in choosing antiemetics:
Vestibular Lesions: antihistamines, anticholinergics and benzodiazepines.
Surgery, chemotherapy, radiation treatment: antidopaminergics and antiserotonergics.


Side Effects and Contraindications 2 3
Potential Side Effects of Antiemetic Drugs
- Sedative Effects
- ranges from drowsiness to severe sleepiness
- Extrapyramidal Signs (with phenothiazines and butyrophenones)
- acute dystonia
- parkinsonism
- akathisia
- tardive dyskinesia
- Neuroleptic Malignant Syndrome (with phenothiazines and butyrophenones)
Use of the drugs mentioned above should be discontinued immediately if extrapyramidal signs become evident; thus you should familiarize yourself with the common symptoms (see table 1). Children are especially prone to extrapyramidal symptoms from the use of antidopaminergic antiemetics (incidence rates of up to 25%); incidence rates in adults are much lower (<1-2%).
TABLE 1. Extrapyramidal Signs| Symptom | Description |
|---|---|
| Acute Dystonia | "Long-lasting contraction or spasm of musculature resulting in abnormal head, neck and/or distal limb or trunk positioning, spasms of jaw muscles, and impaired swallowing"3 |
| Parkinsonism | "Resting tremor, muscular rigidity, akinesia (decrease in spontaneous facial expressions, gestures, etc.)"3 |
| Akathisia | "Inability to sit; complaints of restlessness, fidgety movements, inability to sit or stand still for at least several minutes"3 |
| Tardive Dyskinesia | "Involuntary movements of the tongue, jaw, trunk or extremities. Choreiform (rapid, jerky, nonrepetitive) or athetoid (slow, sinuous, continual) movements."3 |
Neuroleptic Malignant Syndrome is a potentially fatal, neurological disorder. It is most commonly brought on by an adverse reaction to neuroleptic or antipsychotic drugs, or when an antidopaminergic drug is abruptly stopped. The symptoms (among others) include: severe fever, unstable blood pressure, rigidity and autonomic dysfunction. Intensive care and discontinuation of the medication is typically needed.4
Contraindications and Precautions of Antiemetic Drugs
This section is intentionally cursory, as further explanation of pharmacy is not within the scope of this website. Instead, the focus will remain on balance and dizziness, with a brief discussion of contraindications for general awareness.
- Do not take these medications with alcohol
- potential for additive effects
- Use with caution in children and the elderly
- extrapyramidal and sedative effects are more profound in these populations
- Women who are pregnant or nursing should not use these medications
- some of these medications have not been studied in pregnant women
- some of these medications can be passed through breast milk
- Use antidopaminergics with caution in patients with renal disease
- The kidneys are largely responsible for excreting these drugs
- Use chlorpromazine with caution in patients with hepatic disease
- these patients may experience exaggerated CNS effects


Implications for Vestibular Testing
The sedating effects of antiemetic drugs can render patients unable to perform tasks required for oculomotor testing. Poor pursuit and saccade results, as well as inability to task, may be the result of impaired concentration from sedative effects. Drugs that act as central nervous system depressants can also effect vestibular testing, as central pathways will not function properly. For these reasons, it is important to coordinate with prescribing physicians to ensure the patient is not under the influence of these medications during vestibular testing.


- Page References - Click the links below for full citations
- Neuropharmacology of Motion Sickness and Emesis
- Clinical Neurophysiology of the Vestibular System (Third Edition)
- Psychiatric Nursing
- Neuroleptic Malignant Syndrome Information Page
- MedlinePlus Medical Dictionary