Antivertigo Drugs
There are two general types of drugs used to treat symptoms of vertigo, nausea and vomiting: antivertigo and antiemetic drugs. Antiemetic drugs are discussed in the next section. Antivertigo drugs are vestibular suppressants that attempt to control the sensation of vertigo as well as associated nausea and vomiting. Vestibular suppressants are often used in conjunction with antiemetics.
How They Work 1
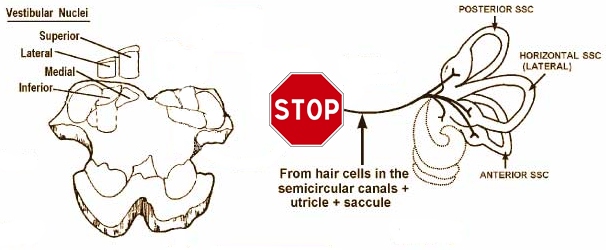
FIGURE 1 (adapted2)
The precise method of action behind many of these drugs is not fully understood; however, the general consensus is that vestibular suppressants act on the neurotransmitters responsible for carrying the vestibular signal from primary vestibular neurons. That is, these drugs seek to block the conduction of impulses from the semicircular canals and otolith organs, before these nerve impulses reach central vestibular structres, and thereby maintain tone in the vestibular nuclei.
- Types of Drugs
- Antihistamines
- Anticholinergics
- Benzodiazepines


Common Uses
Acute Vertiginous Attacks1
The most salient point to consider when using antivertigo drugs to treat acute vertiginous attacks is whether or not the attacks last long enough for the medication to be effective; if an effective blood level is not reached before the attack ends, antivertigo medication will be unsuccessful. This means brief episodes of vertigo, such as BPPV and VBI, cannot be controlled with the use of vestibular suppressants taken at the onset of the attack.
It can take upwards of 2 hours to reach peak blood levels, so acute attacks lasting at least an hour are the best candidates for vestibular suppressants taken at the onset of symptoms. For example, antihistamines need 20 - 30 mintures to initiate action, and reach maximum effectiveness after 1 - 2 hours. Antihistamine vestibular suppressants typically have a half life of 8 hours.
Chronic Vertiginous Attacks1
Patients experiencing frequent vestibular attacks lasting less than an hour are not without recourse. When the episodes are moderate-to-severe and recur often, prophylactic treatment may be a viable short term option. "Short term" must be emphasized, as long term use of vestibular suppressants can impede/slow central compensation (and thus recovery) in two main ways:
- The stronger suppressants have stronger sedative effects, which delay the return to normal mobility, which in turns slows compensation.
- As their name implies, vestibular suppressants "suppress" vestibular signals from the labyrinth, which interferes with the tonic rebalancing inherent to central compensation.
Vestibular suppressants do have their place, however. Patients with acute peripheral vestibular impairment (with vertigo) may require strong vestibular suppressants, but these should be withdrawn gradually once vomiting stops to allow compensation. Such a patient may be switched to milder suppressants to control vertigo throughout the day, coupled with symptomatic use of antiemetic drugs. Because the milder suppressants allow for routine activities, drugs such as scopolamine and meclizine are well suited for motion sickness.
Chronic Dizziness1
Note the preceding two sections specifically state vertiginious attacks. Chronic (or other) dizziness of non-vestibular origin is not appropriate for treatment with vestibular suppressants. Antivertigo drugs cannot control non-vestibular dizziness.


Side Effects and Contraindications 1
Potential Side Effects of Antivertigo Drugs
- Drowsiness
- especially in the elderly
- Withdrawal Symptoms (especially with benzodiazepines and scopolamine)
- dizziness
- nausea
- vomitting
- headaches
- disequilibrium
- general seizures (with abrupt withdrawal of benzodiazepines)
- Habituation and Dependence (with benzodiazepines)
- Altered mental state and hallucinations
- possible with scopolamine use in the elderly
Contraindications and Precautions of Antivertigo Drugs
This list should not be considered exhaustive.
- Do not take these medications with alcohol
- potential for additive effects
- Scopolomine should not be used with children
- side effects are more profound in these populations
- Do not use benzodiazepines in children under 6 months or pregnant or nursing women
- increased risk of birth defects
- Antihistamines are contraindicated in patients with:
- asthma
- emphysema
- chronic pulmonary disease
- difficulty urinating due to enlarged prostate
- All anticholinergic medications should be used with care in patients with:
- glaucoma
- pyloric obstruction
- urinary bladder neck obstruction with intestinal obstruction
- other CNS depressant drug use


Implications for Vestibular Testing
It goes without saying that vestibular suppressants will interfere with vestibular testing; activated end organs will be unable to transmit vestibular signals for central processing. Additionally, the sedating effects of some antivertigo drugs can render patients unable to perform tasks required for oculomotor testing. Poor pursuit and saccade results, as well as inability to task, may be the result of impaired concentration from sedative effects. Drugs that act as central nervous system depressants can also effect vestibular testing, as central pathways will not function properly. For these reasons, it is important to coordinate with prescribing physicians to ensure the patient is not under the influence of these medications during vestibular testing.


- Page References - Click the links below for full citations
- Clinical Neurophysiology of the Vestibular System (Third Edition)