Disruption of Blood Flow
While the previous section covered the vasculature that supplies oxygenated blood to the structures of balance, this section looks at the consequences that arise when that flow of blood is impaired. First we'll discuss the largely reversible damage that can occur following transient ischemia - a reduction in adequate flow of blood to tissue. Next we'll tackle lasting damage due to cessation of blood flow due to blockage of a vessel; this severe, prolonged ischemia leads to "infarction." Last we'll investigate another type of severe ischemia: hermorrhage.
Ischemia and the Transient Ischemic Attack (TIA)
On average, someone has a stroke in the United States every 40 seconds.1 The prevalence of vascular disease is too great to be unfamiliar with its basics. In fact, a Swedish study found that approximately 1/4 of cases of isolated acute vertigo could be attributed to caudal cerebellar infarction.2 It is important to note study participants were admitted to an emergency clinic, meaning audiologists and other clinicians not practicing in such a setting are unlikely to encounter these patients initially. Nevertheless, this information is useful to avoid improper diagnosis of a labyrinthine disorder during vestibular examination. While the labyrinth may indeed be affected, the point of the above-mentioned study is that the true etiology may very well be vascular in nature.
Let's delve in by defining two important terms:
- Ischemia
- Deficient supply of blood to a body part (as the heart or brain) that is due to obstruction of the inflow of arterial blood (as by the narrowing of arteries by spasm or disease). 3
- Transient Ischemic Attack
- A brief episode of cerebral ischemia that is usually characterized by temporary blurring of vision, slurring of speech, numbness, paralysis, or syncope and that is often predictive of a serious stroke—abbreviation TIA; called also mini-stroke. 3
The neurological signs and symptoms of a TIA are generally short-lived, without lasting effects. TIAs are common in the elderly, and are often indicative of more serious ischemic events to come.1 4 To illustrate the import of a short timecourse for recovery from an ischemic event, let's consider the labyrinth. Recall that the inner ear is especially susceptible to disruptions in blood flow as it is supplied by a single end artery without collaterals (labyrinthine/internal auditory). Another factor that renders the labyrinth highly susceptible to ischemic events is the inner ear's high-energy metabolism.4 This sensitivity has been approximately quantified in animal studies, with typical findings showing cochlear potentials decreasing within one minute of ischemia. Cochlear function generally recovers if the ischemia lasts less than 10 minutes. Periods without blood flow lasting 15 to 30 minutes result in outer hair cell loss and permanent cochlear damage.5 Keep in mind different tissues have different time thresholds to induce dysfunction and necrosis of tissue so the timeframes above apply specifically to the inner ear, but the general pattern is universal (i.e., the shorter the ischemic event the better the chances for recovery).
With a little background under our belts, we now consider another important vascular disorder:
Vertebrobasilar Insufficiency (VBI)6
Vertebrobasilar insufficiency (VBI) is a very common cause of vertigo due to ischemia, especially in the elderly population. Common symptoms are described below:
Symptoms
- sudden onset
- several minutes' duration
- vertigo
- nausea and vomitting
- visual field defects*
- diplopia*
- headaches*
- *Symptoms caused by ischemia of the posterior circulation
Notice the symptoms are sudden in onset; this is highly typical of all vascular lesions. It does not take long for sensitive neural tissue to react from inadequate blood flow. Compare this to the more insidious onset of symptoms caused by slow-growing tumors. Thus patient report of sudden onset usually rules out neoplasms and points instead to a vascular etiology.
VBI may produce vertigo alone as an early symptom, but it will eventually be accompanied by other posterior circulation symptoms. In fact, consistent episodes of vertigo without the eventual appearance of the other symptoms listed above are indicative of something other than VBI.
Symptoms can be brought on by atherosclerosis of the subclavian, vertebral, or basilar arteries. Atherosclerosis refers to the buildup of fatty plaque inside arteries, which eventually hardens and narrows the blood vessels. Symptoms are also precipitated by Subclavian Steal Syndrome, though this condition is rare. Subclavian Steal Syndrome results in VBI when blood is siphoned down the vertebral artery, away from the posterior circulation, to supply the upper extremities. Understandably in this case, VBI and its associated symptoms would be brought on by exercising the arms and shoulders. Ischemia of the posterior circulation resulting in VBI can also be caused simply by "looking up" in some patients. That is, when arching the neck back it is possible to "kink" the basilar artery. This can occur from cervical spondylosis, a degenerative disease of the spine. Other triggers may be due to orthostatic hypotension or Stokes Adams attacks which are discussed in the section on blood pressure.
Most often, treatment of vertebrobasilar insufficiency relies on controlling risk factors associated with vascular disease. Common targeted conditions include:
- diabetes mellitus
- hypertension
- hyperlipidemia
Antiplatelet drugs, such as Aspirin, are often effective in milder cases. In more severe cases anticoagulation drugs, such as Warfarin/Coumadin, may be needed. This is especially the case if basilar artery thrombosis is suspected. We will learn more about thrombi further down the page.


Infarction and Ischemic Stroke
The word "infarction" is recognizable to many from daily life. The term "myocardial infarction" referring to a heart attack has become fairly popular vernacular. However, what exactly is an infarction? The definitions below will clear this up before moving on.
- Infarct
- An area of necrosis in a tissue or organ resulting from obstruction of the local circulation by a thrombus or embolus. 3
- Infarction
- The process of forming an infarct. 3
An infarct is damaged tissue from a lack of blood flow. It is important to understand the relationship between infarction and ischemia (mentioned above). Namely, infarction occurs due to ischemia, or put another way, tissue dies when it does not receive proper irrigation. Infarction can occur from ischemia caused by two types of vascular blockage: a thrombus or an embolus. A thrombus is more commonly known as a blood clot, and is attached to a blood vessel's wall. Conversely, "embolus" refers to a particle which circulates through the blood. These types of arterial occlusion are the etiology behind "ischemic stroke," which accounts for 87% of all strokes.4
- Embolus
- An abnormal particle (as an air bubble) circulating in the blood. 3
- Thrombus
- A clot of blood formed within a blood vessel and remaining attached to its place of origin. 3
Neurologists train for years to determine the site of vessel blockage by considering the intricate map of arteries and the structures those arteries supply. While this in-depth understanding and diagnostic skill is well out of the scope of this website, we will tackle some big picture site-of-lesion considerations that will shed some light on common (and some not so common) disorders of balance. We have already discussed the pertinent vasculature of the structures of balance, and will now examine various sites of arterial blockage and how the ensuing infarction can affect your patients.
Infarction of the Brainstem 6
Stroke syndromes associated with the posterior inferior cerebellar artery (PICA) and anterior inferior cerebellar artery (AICA) are common, and result in damage to the brainstem and/or cerebellum. The tables below summarize the major signs and symptoms produced by occlusion of the PICA and AICA.6
TABLE 1.
| Symptoms and Signs |
PICA Infarct |
| Vertigo, Nystagmus |
Vestibular nuclei, posterior inferior cerebellum |
| Tinnitus, hearing loss |
N/A |
| Gait and limb ataxia |
Ventral spinocerebellar tract, posterior inferior cerebellum |
| Dysphagia, decreased gag |
Vagal nuclei and nerve |
| Facial hemianesthesia |
CN V and nucleus |
| Facial paralysis |
CN VII |
| Crossed hemisensory loss |
Spinothalamic tract |
| Horner's syndrome |
Descending sympathetic fibers |
Note that vertigo caused by blockage of the PICA follows the artery's supply: for instance, the vestibular nuclei reside in the medulla of the brainstem, which is supplied by the PICA. Correspondingly, vertigo is produced by lesioning of the vestibular nuclei and/or posterior inferior cerebellum - not by affecting the vestibular apparatus/inner ear directly. Also residing in the medulla is the nucleus of CN X, the vagal nerve. Damage to this nerve can result in dysphagia and a decreased gag reflex. Auditory symptoms are absent, as again, the labyrinth is unaffected.
- Ataxia
- An inability to coordinate voluntary muscular movements that is symptomatic of some nervous disorders. 3
- Dysphagia
- Difficulty in swallowing. 3
- Horner's Syndrome
- A syndrome marked by sinking in of the eyeball, contraction of the pupil, drooping of the upper eyelid, and vasodilation and anhidrosis of the face, and caused by paralysis of the cervical sympathetic nerve fibers on the affected side. 3
TABLE 2.
| Symptoms and Signs |
AICA Infarct |
| Vertigo, Nystagmus |
Labyrinth, vestibular nerve, flocculus |
| Tinnitus, hearing loss |
Cochlea, auditory nerve, cochlear nucleus |
| Gait and limb ataxia |
Middle cerebellar peduncle, anterior inferior cerebellum |
| Dysphagia, decreased gag |
None |
| Facial hemianesthesia |
CN V and nucleus |
| Facial paralysis |
CN VII |
| Crossed hemisensory loss |
Spinothalamic tract |
| Horner's syndrome |
Descending sympathetic fibers |
Contrast table 2 with infarction due to occlusion along the PICA. While vertigo is still a prominent symptom from AICA occlusion, its etiology has changed. Remember that the AICA often gives rise to the labyrinthine artery, which is the sole supply of oxygenated blood to the inner ear. Thus, vertigo is precipitated due to lesioning of the labyrinth (and/or vestibular nerve and cerebellar flocculus). That means hearing loss and/or tinnitus (i.e., auditory symptoms) are present along with the vertigo because the vestibular apparatus, cochlea and CN VIII are all supplied by the AICA via the labyrinthine artery. Additionally, dysphagia and decreased gag reflex are absent, as the AICA does not supply the medulla.
These differences in symptoms based on which structures each artery supplies allows us to make some general conclusions about the site of lesion. Let's consider these differences in two common syndromes brought on by occlusion of the PICA and AICA.
Lateral Medullary Syndrome (Wallenberg's Syndrome) 6 7
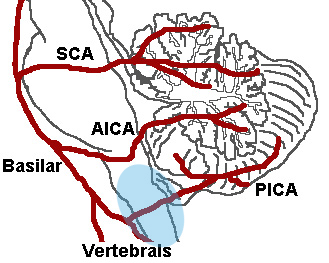
Wallenberg's Syndrome is a very common condition, resulting in infarction of the lateral medulla. While this may lead to the assumption the occluded vessel is the PICA, this is rarely the case; instead, the vertebral artery is typically the site of lesion. However, this still causes infarction of the structures supplied by the PICA, because the PICA arise from the vertebral arteries (see figure 1). There are several characteristic symptoms and signs of lateral medullary infarction:
FIGURE 1
Wikimedia Commons
Symptoms
- vertigo
- diplopia
- dysphasia
- dysphonia
- ipsilateral facial pain
Signs
- ipsilateral Horner's Syndrome
- loss of pain and temperature on the lesioned-side of the face
- ipsilateral paralysis of the throat
- ipsilateral lateral rectus and facial weakness
- ipsilateral dysmetria, dysrhythmia and dysdiadochokinesia
- spontaneous nystagmus
- loss of pain and temperature sensation on the side of the body opposite the lesion
Does this sound familiar? These signs and symptoms are the same as those listed in table 1 above (PICA Infarct). This should drive home that knowing the major vessels and what tissues they supply can be extremely useful in differential diagnosis. Keep in mind not all of these symptoms will be present in every patient, as the severity of the syndrome is predicated by the extent of the damaged tissues (i.e., the size and location of the lesion). Some patients will experience lessening symptoms in a few weeks or months (less common), while others will experience difficulties for years (more common). Both diagnosis and prognosis are left to the neurologist, but recognizing these signs and symptoms can prove useful in predicting and interpreting your own test results.
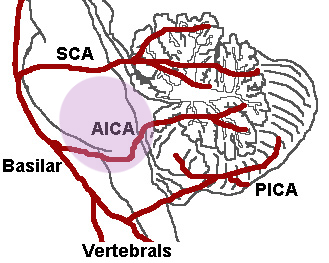
Lateral Pontomedullary Syndrome 6
As we learned above, occlusion of the AICA can affect the pontomedullary area and parts of the inferior cerebellum. The middle cerebellar peduncle is often the area most affected. As we saw with Wallenberg's Syndrome above, the signs and symptoms of lateral pontomedullary syndrome are easy to intuit based on the structures supplied by the AICA (see figure 2).
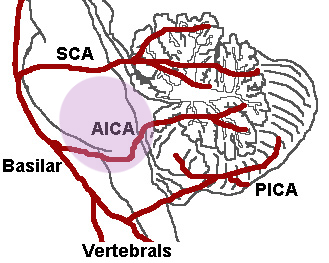
FIGURE 2
Wikimedia Commons
Symptoms
- severe vertigo
- nausea and vomiting
- unilateral hearing loss
- tinnitus
- facial paralysis
- poor coordination (asynergy) of the cerebellum
Signs
- ipsilateral hearing loss and/or tinnitus
- (labyrinth and auditory portion of CN VIII)
- spontaneous nystagmus
- (labyrinth and vestibular portion of CN VIII)
- ipsilateral weakness of the face
- ipsilateral cerebellar dysfunction
- (anterior inferior cerebellum)
- ipsilateral loss of pain and temperature sensation on the face
- contralateral loss of pain and temperature senstion on the body
- (crossed spinothalamic fibers)
As described above, we see auditory signs can occur with occlusion of the AICA, and the cause of vertigo is labyrinthine. While the residual effects can gradually improve over time, the vertigo may last for weeks or even months due to damage of central compensation structures.
Infarction of the Cerebellum 6 8
The cerebellum plays an integral role in motor control and timing, having profound effects on eye movements, speech, limb movements, posture, and gait. You can learn all about the cerebellum by visiting its section in this website. For now, the focus will be on the consequences of cerebellar infarction.
To start out, let's expose cerebellar ischemia's potentially deceptive behavior: infarction can be isolated to the cerebellum, without affecting the brainstem. How is this deceptive? Consider the symptoms of infarction isolated to the cerebellum:
Symptoms
- severe vertigo
- vomiting
- ataxia
These symptoms, without the presence of brainstem signs (discussed above), can be confused with an acute peripheral/labyrinthine episode. Characteristics that help identify cerebellar infarction as such include gait ataxia, limb ataxia, and gaze-evoked (gaze paretic) nystagmus. Of course the best method to reveal cerebellar infarction is with an MRI scan.
With above caveat in mind, let's turn back to potential sources of ischemia. If you recall the arteries of the posterior circulation, the following vessels are no surprise:
Arteries of Isolated Cerebellar Infarction
- vertebral artery
- posterior inferior cerebellar artery (PICA)
- anterior inferior cerebellar artery (AICA)
- superior cerebellar artery (SCA)
As discussed above, occlusion of these same vessels can also lead to brainstem infarction. When a lesion affects both the brainstem and the cerebellum, both types of signs and symptoms will be present. Clinically, it is easy to imagine the potential severity of such an event.
Another point to keep in mind is the potential of cerebellar swelling following an ischemic attack. After a latent period of 24 to 96 hours it is possible for the cerebellum to become swollen enough to begin causing progressive brainstem signs. The result, if unchecked, leads to quadriplegia, coma, then death. Surgical decompression surgery is required to alleviate this condition.
Infarction of the Labyrinth 6
Familiarity with the blood supply to the inner ear is essential to understanding stroke syndromes affecting the labyrinth. However, just as with the rest of the posterior circulation, after the blood supply is mastered the signs and symptoms follow naturally and are easy to remember. Keep in mind the following usually occurs in the elderly population with a history of vascular disease, stroke, TIA, etc.
Sudden unilateral hearing loss and severe vertigo can be caused by ischemia of the labyrinthine artery. Because the occlusion would occur before the artery divides, both vestibular and cochlear structures are affected.
Sudden hearing loss without vertiginous symptoms can be attributed to ischemia of the common cochlear artery or one of its branches.
Vertigo without hearing loss can be due to infarction of the vestibular labyrinth due to occlusion of the anterior vestibular artery. The vertigo can last minutes or even days depending on the severity of the lesion. The clinical description is "sudden, severe vertigo without hearing loss or brain stem symptoms". 6
Although benign paroxysmal positional vertigo (BPPV) is covered in depth elsewhere, it bears mentioning here, as BPPV is a possible sequela following an ischemic attack involving the anterior vestibular artery. Infarction of the macula of the utricle can cause the release of its otoconia into the posterior semicircular canal. The posterior canal can still generate vertigo due to the fact it may still be intact, as it is supplied by the common cochlear artery.


Hemorrhage and Hemorrhagic Stroke
Content coming soon!